This article is obviously inspired by recent . . . “events!” I wanted to bring something to readers that would help all of us navigate a difficult period with more confidence, safety, and security, even though we’re dealing with a rapidly changing landscape with Coronavirus. So . . . No pithy intro or exit. Let’s get on with discussing this health matter with a veteran in the medical industry.
(This article ran in AGENDA April 2020, Issue #12. Get the magazine in print or digital form.)
Melanie Wise: Can we give readers your working background?
RN: I’m am an RN (Registered Nurse). I’ve been an acute care nurse for 16 years.
Melanie: To the lay person, what does that mean?
RN: It means I work in hospitals with sick people and those at risk for dying as compared to nurses who work in doctors offices or clinics. It means nurses can do a lot of different things. Not all of them work in hospitals, facing acute and/or emergent conditions.
PRECAUTIONS YOU CAN TAKE: Masks
Melanie: If people are going to use a mask, can you explain the proper way of actually using it, putting it on, taking it off, etc.
RN: For paper masks, they are not going to give you a great seal, most of them have a little pliable band on the nose part where you use two fingers to mold to the shape of the nose. The mask you are using: just assume that it is dirty on the outside. So don’t touch it. Go behind your ears and grab the little band behind your ear and you can take it off from there without actually touching the mask. And remove it slowly. Don’t rip it off your face, because that’s going to disturb the molecules. Move it off and away from your body. You can also remove them under the chin, reaching inside the mask with one finger. But do not touch the outside, because then your hands are contaminated. If you do touch the mask, wash your hands immediately after.
Some people have been putting the mask down to talk to someone, to eat or smoke and that defeats the whole purpose of wearing it to begin with.
Melanie: And most of the paper masks are designed for single use, right? That means you put it on, you take it off, you throw it away.
RN: Yes, but in these times, the hospitals can’t even do that. They’re told to use one per shift. Someone asked, because in other countries they don’t have the supplies, so the doctors have been going home and washing the masks at the end of each shift and letting them air dry and then using them again the next day. Bleach kills the bugs, but I don’t know how that affects the masks, if it degrades it. As far as I know, no one has been in this predicament.
Distance
Melanie: Could you explain the difference between airborne and droplet and what does that mean?
RN: So droplets tends to be “heavier” molecules and in open air they fall quickly to the ground. The droplet precautions we had in the hospital before the COVID-19 was you had to wear a mask, and if you were within 3 feet of the patient, you would wear a gown. Gloves are worn in all circumstances.
Airborne is tougher. In cases of tuberculosis, it can be highly contagious and can travel further in the air because it’s a lighter molecule. You need a respirator. You need a mask that makes a seal so you’re not breathing anything out beyond the mask and you’re not breathing anything in beyond the mask.
Melanie: The mask is essentially an enclosed system.
RN: Yes.
Melanie: The coronavirus is droplet, not airborne.
RN: I call it enhanced droplets,because they want us to wear goggles to protect our eyes.
Melanie: For the general public . . .
RN: The CDC is saying to use droplet precaution, and to protect your eyes with goggles or a mask that covers your whole face.
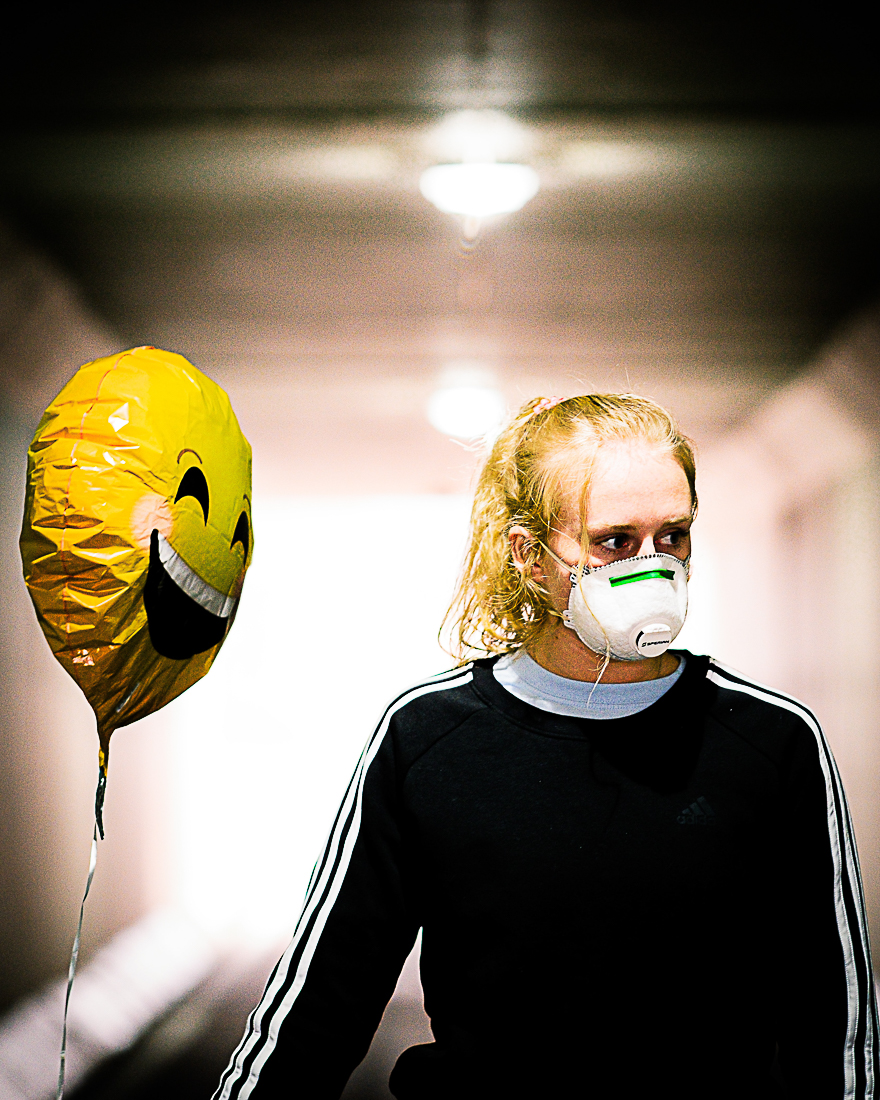
Melanie: For the average person, the masks that everybody is wearing, are they adequate for droplets and/or airborne?
RN:It’s not adequate for airborne,but adequate for droplet . . . if you maintain distance as well. The CDC is saying keep a distance of 6 feet.
Hand Washing
Melanie: Tell us about washing your hands.
RN: It’s not just washing your hands, but doing it correctly. Washing every inch of your hands. Washing for 20 seconds at a minimum. Scrubbing every surface under your nails, around your fingers, the base of your fingers, around your thumbs, your wrists. I haven’t watched a lot of people wash their hands, but in a hospital, there’s a procedure.
Sixteen years as a nurse, the majority of those patients don’t wash their hands well if they wash them at all. If they do, they put their hands under the water for a second and have soap on it for maybe a second if they even do the soap.

Melanie: And you’re speaking of the average person washing.
RN: I’m speaking of the average person who has not inquired about it or I’ve tried to teach them how to wash their hands properly. I am usually confronted with,”But, I’m not dirty.”So it’s a perception of–and maybe it’s a difficult thing–people don’t like to be known as dirty. It’s not a judgment. We use our hands for everything, and you know, money is dirty. Most people don’t wash their hands after using money. You don’t think about it since it is something you handle everyday,you don’t think about it.
Melanie: So moms with kids actually have to be careful about touching their kids, too, right?
RN:Yes and no. You have a baby, you’ve got to touch the baby. There’s no way around that. That doesn’t mean you shouldn’t love on your baby. The one good thing with families is you don’t have to worry about social distancing as much. They are talking about out in the world. You can’t social distance yourself from your kids or your babies. Grandma and grandpa might need help, but maybe just wash your hands a lot and cover your mouth, cough into your elbow. Don’t touch each other so much. But if you wash your hands, you should be okay.

Additional Safeguards
Melanie: Since there is no western medical cure for viruses, does it make sense for people to engage in practices that boost natural defenses? If so, what would you suggest?
RN: Yes, it certainly can’t hurt. Lowering stress is very important, because high stress is the largest tax to the immune system. Eat well, hydrate, make use of Vitamin C, Zinc, and other supplements.
I get nervous about suggesting these particular things because people will blow off the other physical precautions/protections that are needed. Yes, boost your immune system, but also be smart about social distance, hand washing, etc.
Melanie: I’ve seen a lot of people out buying antibacterial wipes and the like, and maybe I’m wrong here, but antibacterial products are not going to deal with a virus. Is that correct?
RN: Yes. They say for this virus to use hydrogen peroxide. Bleach, of course, kills a virus. My understanding is this contagion can last up to three hours on surfaces.
CORONAVIRUS SYMPTOMS AND RISKS
Melanie: Got it. Let’s go over the basics. What are the symptoms of coronavirus?
RN: Fever, cough, fatigue, a temperature, malaise, and body aches. Some people have diarrhea, not a lot.
Melanie: Can you explain what the major risks are?
RN: People that are Immunocompromised that have a medical history, chronic conditions, like immune diseases or lung issues like COPD; heart issues like heart failure are more at risk. It’s also difficult with kids and babies. They are high risk like the elderly. Anyone over 65, because in general, they are the population that don’t have good stamina or the reserves to handle this kind of sickness.
High fever dehydrates you, and with malaise and fatigue you may note at as much or drink as much. Reserves get depleted quite quickly, and that’s how they get so sick so fast, whereas an average healthy 25-year old is just going to feel yucky for a couple of days then be okay. Drink some Gatorade and be okay. Because their bodies have there serves to recover from fighting a virus and getting over it,where as someone who doesn’t have those reserves is not going to be able to do that. They’re going to need help.
People that are compromised, develop complications like fluid in the lungs and shortness of breath; they can’t breathe. When the lungs fill with fluid, they get in trouble. These complications can develop into some form of pneumonia.

Melanie: And are there age ranges that are specifically at risk or is it just if you have any of those symptoms/diseases that you just mentioned, or is it combined with age?
RN: Yeah, they’re saying anyone over 65 and babies. I’m not sure of the age for the kids, I don’t have much info on the kid thing, because I deal with adults. But anyone over 65, and in general anyone with medical history that could put them at risk. All those other things I mentioned before.
Melanie: In a nutshell, if you have health situations that are less volatile or . . .
RN: No, not necessarily because someone with cerebral palsy or muscular dystrophy can be high risks as well, because that attacks the muscles. And if it’s attacking the muscles that dictates breathing, it could affect breathing, which is going to cause a struggle.
Melanie: It’s a serious situation, but I wanted to focus on actionable data so that people can possibly dial down their fear level a little. So with that in mind, in terms of the risk factors you just outlined, would that be the same factors as an average flu?
RN: Yes, of course.
Melanie: Let’s consider just your average person – someone who doesn’t have a preexisting conditions getting the virus. That’s basically a situation where you have the flu for a couple of weeks and you’re done, right?
RN: Not even for a couple of weeks. I think the average is nine days, and I think healthy people don’t even have it that long. 3-5 days, something like that, if that . You’ll feel crappy.
SIMILARITIES TO AN AVERAGE FLU
Melanie: What are the similarities or differences between the coronavirus and the average flu?
RN: They are both viruses, so we can’t cure them. We don’t have that capability yet. Because we don’t have a cure for the flu, all we can do is treat the symptoms. Because they are both viruses, they have similar symptoms. I guess the rub with this one is that it just seems to be so prevalent and so fast. And for the amount of time it has spread, we probably don’t even know to what degree, the health care industry is revving up for the worst.What we’re seeing is not the worst yet, at least in the USA.
Dealing with Coronavirus is new, so we don’t necessarily have the testing down perfect, or there are so many people being tested it’s backlogging so it takes up to five days for someone to find out if they have the virus. And those people have to be isolated for those five days. No matter what mainstream media says, we do not know how long coronavirus has existed. But [we’re] dealing with this virus in its infancy, so it’s hard to figure out what’s going to happen as we get to the “teenager” age.

Get Good Data
Melanie: In terms of just good reliable, no nonsense data, where are you finding your data?
RN: The CDC, the Center for Disease Control. There’s a lot of local governmental sites by area that are getting their information from the CDC so that should be okay. Or WHO, World Health Organization, their website can be pretty good, too.
The theory being you’re getting the information from the horse’s mouth as opposed to someone who thinks they know what they’re talking about . . . and they may or may not.
Melanie: Got it. And is our mainstream media covering the details of safety or precautionary measures accurately?
RN: It’s hard for me to say, because I don’t watch a lot of them. It would be too much info, and a lot of it – I don’t know what the word is – because news is so dramatic. Because it really is a dramatic situation. It’s hard not to take drama from that. A lot of the news coverage is just telling you what they’ve seen or heard, but that doesn’t mean it’s fact.
The only thing I can equate it to is if I watch a medical show, I’m going to see all the things that don’t happen in real life, because I know what happens in a hospital. When the average Joe doesn’t know that, it looks good on TV, and it’s dramatic, so they don’t question it. How would they know what to question anyway? But when I watch, I say, “Ugh, it doesn’t work that way!”
Moving Towards Health
Melanie: In terms of the percentage of population infected, it is spreading fast, but it is—please correct me if I’m wrong, and based on what you and I discussed previously—actually a very small percentage of the population that has actually been infected. Is that correct?
RN: Yes. In terms of population, only a fraction of a single percent of people actually have the virus. And in the US, dealing with coronavirus is new. We haven’t gotten to that phase yet where everyone who is going to be exposed has been exposed, and add to that, it’s two weeks later before they discover they’re sick. So the numbers of new cases will continue to rise.

The good news is China is 88% recovered, which is great and gives us hope. And the vast majority of cases, (approximately 80%) are mild cases. That would mean that they have figured out how to contain it [to be able] to minimize its spread. When I’m looking at this one site and it says 88% recovery for China, they say 1% for the USA.
Remember I said the dealing with the virus is kind of in its infancy. For China, dealing with the virus is much older. They are further along in the lifetime of dealing with the spread of the virus. It still exists of course, but we are seeing a positive change in new cases/spread in China.
RECAP
Melanie: Is there anything you can say to give people just a little sense of security or safety?
RN: Just be smart about it. Nothing wrong with washing your hands. Social distancing for strangers, I mean your family is your family. If you feel sick by all means don’t go see grandma and grandpa. Don’t kiss the baby. Be mindful. If you have a fever, self-quarantine.
We’re still within our 2 weeks zone (interview took place on March 19,2020 and business modification, school closures, etc. has occurred on approximately 3/17/20 in LosAngeles). It takes two weeks for people to get symptoms, so we’re still within those two weeks of saying,“Hey people, you all need to stop doing what you’re doing.” You know what I mean? That’s another reason why the number of cases are still getting bigger.
Melanie: Is there anything you think we may have missed?
RN: It is a tough subject, because it’s changing hour by hour. I don’t feel like I can talk about this with total confidence, because it’s just too soon, and I know hindsight is 20/20. But really, the rule of thumb always is wash your hands; don’t touch your face; be mindful of what you’re doing; don’t share your drink with someone.
It’s not always about the person. It’s not always just about you. You have to think about the other people in the world, too. You’re young, you feel good. You can’t imagine something hurting you, but you could be giving something to someone that does hurt them. So it is time to not be selfish. And I know mass hysteria leads to incredible acts of selfishness . . . these people think they are in survival mode, but it doesn’t have to be that bad if we all just take care of each other.
Melanie: You’re right. Thank you so much.
RN: You’re welcome.
This article ran in AGENDA April 2020, Issue #12. Get the magazine in print or digital form.




